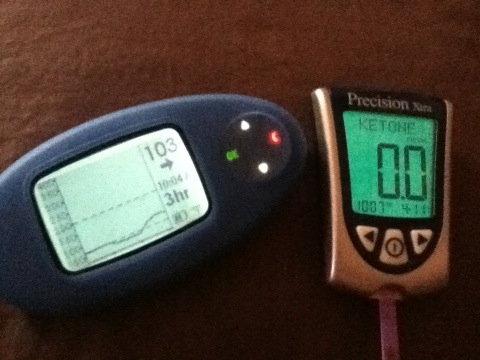
At times like now when I am sick, I am so very grateful for these devices.
Category Archives: BG
Too Much to Ask?
I’ve posted before about the lack of glucose meter accuracy and if we’re friends on Facebook, you’ve seen pictures I’ve taken comparing meter results. When I was using the One Touch Ping meter that worked with my pump, I had issues with it giving me false low readings. Luckily I have the Dexcom CGM so in seeing the discrepancy between meter and sensor readings, I would retest to get a higher reading. One Touch was very accommodating and sent me a new meter which solved that issue. Mostly. At the time my CDE suggested I try the Freestyle meter which I did and switched for some time to primarily use the Freestyle Lite. I did many comparisons between the two meters with the same blood sample and got substantial differences. I put a stop to that pretty much for my own sanity. In the end I stuck with the Ping meter mainly for convenience of the remote bolus function with my pump and also being a long time One Touch user.
Then, two months ago, I switched to the OmniPod system and the Freestyle PDM became my primary meter since it also functions as the manager to all insulin dosage functions. In that same time period, I purchased the new One Touch Verio IQ meter. Although the Verio is not my primary meter, I do like it a lot. Of course I have done some reading comparisons between the two. And I’m back to getting very considerable differences.
A couple of weeks ago I read a post by Mike over at Every Day Ups and Downs. He had reviewed the new iBGStar meter from Sanofi. In his review, he noted that the iBGStar was giving him readings higher than other meters (Accu-chek Expert and Contour Link). In posting his results, he got confirmation from Sanofi that “the iBGStar has been developed to give readings which are automatically corrected against Haematocrit* and plasma values. Both of these corrections can mean that your new iBGStar monitor may give readings higher than you are used to. If you have any concerns over what this change of readings may mean, we would advise you to consult your doctor or other healthcare practitioner for further training.” This made me wonder if the new Verio has been developed similarly.
Also, a few days ago I read a post by Adam over at diaTribe, reviewing the new meters on the market, including the Verio. In his findings, the Verio had 100% accuracy with results under 75 mg/dL and 95% accuracy with results over 75 mg/dL compared to lab readings. That is some pretty solid findings. It also made me wonder about my own comparisons using the Verio.
While I appreciate all the new technology coming out or being worked on – mySentry, Telcare, AP, etc. and think they are hugely beneficial to the lives of those living with diabetes, what I want the most is a BG meter that will give me results I can rely on. One that will not be just plus or minus 20% of my actual BG. My next endo appointment is in 3 weeks and I plan on taking both the PDM and Verio meters to be tested at the lab. If the Verio results are indeed more “accurate”, as much as I wouldn’t want to, I would consider changing it to my primary meter. It will be an inconvenience in some ways but may be worth it if it means trusting the results more.
FDA and BG meter companies – without accurate BG readings, all else in our management means nothing. I can eat all the right things, count every last carb, test 20 times a day, exercise every single day and dose the most precise amount of insulin. But if my readings aren’t accurate all of those other things will not help me keep my diabetes in control. I can’t help but wonder if this is the very reason I cannot seem to get my a1c under 7. My BG levels may not actually be what they seem. And that to me, as a person with diabetes, is a huge problem.
Sick or Not.
I haven’t been feeling well for going on two weeks. Not exactly sick but not well. When you have diabetes, any little ailment or ill feeling causes more questions and concerns than normal. And I hate that. Things like the sniffles or a little dizziness or some fatigue can be brushed off by a person without diabetes if they choose. But when you have to worry about your BG as well as the feeling you are experiencing, it’s a whole different ball game. Your mind begins to wander about the cause of your suffering. Could I be starting with another auto immune condition? Could it be complications? Is it diabetes related at all? To determine if your high BG is being caused by not feeling well or if not feeling well is being caused by your high BG is next to impossible. Not to mention making sure ketones aren’t part of the scenario. It can all be a bit overwhelming.
As for what has been ailing me, I’m hoping to find out. I’ve already had a couple of things ruled out and have a few appointments scheduled in the coming week. I have a feeling most of my symptoms could very well be allergy related believe it or not. And if that’s all it is, I can deal with that. I really just want to feel back to normal already. Especially to get back to working out. (did I really just write that??) But I take not feeling well very seriously. Maybe too seriously? And I can’t help but place the blame for that on diabetes.
Wordless Wednesday.
Scary Days.
Low blood sugars don’t normally scare me. Sure I’ve had times where I have felt unwell enough to be a little concerned but generally speaking I don’t have a great fear of them. I don’t feel the urge to eat everything in sight to treat a low. I stick to my juicy juice box or maybe a soda or glucose tabs if I have nothing else available and I’m usually good in a reasonable amount of time. It could be because I’ve (thankfully) never lost consciousness, I’m not sure. I’ve also never lived alone. I went from living with my parents and sister to living with my hubby.
Two weeks ago however, I had an incident that had me in tears from fear. I was working from home so was alone in our apartment. It was not quite 2 hours post breakfast that the reading on my Dexcom caused me some concern.
I checked with my meter and confirmed I was actually dropping that much with a 76 mg/dL. I grabbed a juice box and also decreased my basal by about 50%. The double arrows on the Dexcom went away but I was still dropping. About 35 minutes, this is what I saw.
I started to get nervous at this point. Less basal, juice and I was still dropping. And feeling completely fine. That is what scared me the most I think. I have not been feeling my lows at all lately and I was afraid that since I wasn’t feeling low that all of a sudden I was going to be low enough to not be able to help myself. So I suspended my insulin and had another juice box. Another 15 minutes later I was still dropping.
I don’t know if it was the fear or the actual low but I started not to feel well. And so I got even more panicked. I decided to get the glucagon out and gave myself a shot in the leg. I didn’t know if I was overreacting but at the moment, by myself, it seemed like the right thing to do. I also thought I was going to regret it with BG in the 300’s but guess what? About 2 hours later, finally, I peaked at 165.
I was never so scared. I was never so relieved. I was never so thankful to have the right tools to help me monitor this blood sugar. I can only imagine what could have happened in this situation when I was first diagnosed 30 years ago without even a glucose meter to test with. Most days diabetes isn’t that scary. But some days it can be very scary.
I Like When Change is Good.
I have made two rather major changes to my diabetes management recently. And I can’t say for sure if it’s one or the other, or a combination of both, but I have seen improvements in my overall BG readings. Which of course is a good thing. For the first time in my insulin pumping life (5+ years) my CDE reduced ALL of my basal rates. Each and every eight of them. That has never happened since I’m on the pump. I wasn’t sure how I felt when I left her visit. I wasn’t exactly experiencing way too many lows. But there have been hours at a time in the past couple of weeks where I’m stuck around the 70-80 mg/dL range. And the lows I have had, she was able to trace to too much basal insulin. So I thought the worst that can happen is I run high and change them back. Right?
Well my first day on my new basal rates have resulted in readings of 60, 99, 112, 152, 142, 115, 106 and 122 mg/dL so far, with the Dexcom line to go with it. I am pretty surprised actually. I guess the reductions may not be too much like I thought! Props to M 😉
So what are these changes you are probably wondering? Switching from Novolog to Apidra insulin and from a tubed pump to the OmniPod. Now your guess is as good as mine why the OmniPod would better control my BG. My guess would be that there is no tube for the insulin to go through so a more direct delivery into my system? No kinks or bubbles from tubing? An angled infusion set as opposed to a straight one? Has any of this been proven? Not that I know of. But for some reason it seems to be working better for me. The Apidra has improved my postprandial (post meal) numbers. My current endo, as well as my previous one, felt there wasn’t much difference between Novolog, Humalog and Apidra. But according to their website “Apidra® works quickly to help control mealtime blood sugar ‘spikes’. You can take Apidra® rapid-acting insulin within 15 minutes before your meal, or within 20 minutes after starting a meal.” I had tried Apidra once about a year ago or so and didn’t stick with it for some reason. But this time I paid more attention and tracked the difference it has made.
Whatever the scientific reasons behind these changes improving my BG results, I truly hope it continues. I’d really love to see an improvement in my A1c in April.
*please keep in mind that I am in no way stating that taking Apidra or using the OmniPod will improve everyone’s diabetes management – don’t forget – your diabetes may will vary*
Feel Good Friday.
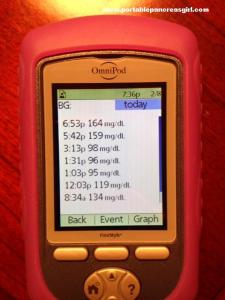
It’s been a long week (even though I only worked four days of it) but it’s Friday. And that makes me happy. I’m all hooked up and running on the OmniPod since Tuesday night. And readings like the ones in the picture make me feel good. I’m even due for my first pod change tonight since using my own, new system. And I’ll have to remember that putting it on my lower right back is not a good spot since that is where my heavy tote bag lies when carrying it. You live and learn!
I wish you all a great weekend 🙂
Impressions.
It’s been 6 days using the OmniPod insulin pump system for a trial period. After the first few hours, I had a very positive first impression. I am going to share what the following days have entailed as I know a few people have shown interest in my experience.
The first pod that I had placed on my back was scheduled to expire Friday evening. That morning as I was riding the railroad to work, I noticed the batteries in the PDM were running low so thought I’d change them while I thought of it. (I never let the batteries on any of my devices, diabetes or not, run all the way out) After putting the new batteries in, the PDM asked me to reset the date and time. I didn’t think this was odd at first but then it told me that a pod deactivation was required. No bueno. Especially on the train. I didn’t exactly know what was going on so in a panic, I texted Cherise who told me that it wasn’t normal for the PDM to do that during a battery change. That made me feel better. A little. Since the PDM wasn’t allowing me to do anything else but deactivate the pod, that’s what I did when I got to work. Luckily I had another with me and began the process to activate and insert a new one a bit earlier than planned. This one I put on my right hip. I went through the insertion process with no issues and the rest of the day went fine. I also confirmed with the OmniPod CDE that this indeed was a fluke and should not happen.
Saturday afternoon, my BG started to rise for no obvious reason. I checked the pod and saw a tad bit of blood around the cannula location. After a few hours of rising BG, unsuccessful corrections and increased basal I decided to change the pod thinking that the absorption wasn’t fully working. I wanted to try my arm this time so that’s where I put this pod. I kept my basal increased for 2 hours or so but my BG wasn’t budging. Patience? Yeah I don’t have much of that, especially when it comes to high BG. I figured the arm site wasn’t working either (it was always hit or miss for me with infusion sets) and changed the pod yet again. Since it was around 10pm and I was planning on going to bed soon, I chose my abdomen since I know I have no absorption issues there. My BG came down nicely overnight. Even a bit too much since I woke up low. I was happy that the pod was apparently working. Until around noon when my BG shot up to around 300 mg/dL for no obvious reason. Since this doesn’t happen to me too often my first thought was that it was a pod issue. But I didn’t want to jump the gun and change it yet again. We went to a friend’s to watch the NFL playoffs and I went toting all my usual extra diabetes supplies plus my Ping pump and accessories. Just in case. Well things worked well and they still are going well. So I’m inclined to now think it wasn’t a pod issue causing yesterday’s BG spike. Saturday’s maybe since there was a bit of blood involved. But I’ll probably never know for sure.
I have one pod left, with my current one scheduled to expire tomorrow night. I’m really hoping to see this one through to its timely ending. Overall I really like the system. Being tubeless is actually better than I even imagined. I keep feeling for my pump in my pockets and it’s not there! It honestly feels like I have lost a part of me. But in a good way. I have to say the only drawbacks that I see are the size of the pods and the speed of bolus delivery like I mentioned originally. More on those …..
The Ping pump delivers boluses very quickly. The normal setting is 1 unit every second or the slow setting, which I use, is 1 unit every 4 seconds. The Medtronic pump delivers at a slower rate of 0.15 units per second from what I’ve found online. I believe the OmniPod CDE told me the pod delivers 1 unit every 40 seconds. That’s a big difference. Now is one rate better than the other? I’m not sure. How I notice the difference is when I’m thinking of eating, I would have to pre-bolus more so with the pod. Not really a deal breaker but something to consider.
Since infusion sets are so small, there are more options in terms of placement. With the pod, since it’s bigger and more bulky, placement needs a bit more consideration. I haven’t hated having them on my body though which is a good thing. I think it’s something to get used to. I feel that not being tethered may truly outweigh this slight incommodity.
Also, I know the fact the OmniPod does not factor in bolus for food when calculating insulin on board (IOB) poses an issue for some. I’m not quite sure how I feel on this one. Many times when the Ping would calculate me to take no insulin for either additional food after eating something prior or a correction within my set active insulin time frame, I would override the calculation to give some insulin. Without taking too much and causing a low BG. For me, OmniPod’s feature seems to be okay.
I’m going to make my decision in the next few days. I’m very glad to have had this opportunity to trial the OmniPod. I would highly recommend the same to anyone who may be considering it. A special thanks to Leighann, Cherise, Penny and Scott for helping me out when I had questions. Or issues. Or was panicking. 🙂
*Once again, OmniPod had no part in this trial of their product or of my impressions using it.*
Please Make It Stop.
Last night I did nothing out of the ordinary. We had dinner of leftovers around 5:30pm and I finished an elliptical workout around 7:45. My BG was 153 mg/dL pre workout and 131 afterwards. Pretty good in by book. I took a shower around 9 and noticed on my Dexcom that I had dropped a little below 100 mg/dL. Still pretty good. I had some tea before getting ready for bed and was in the living room while my Dexcom receiver sat in the bedroom. I got back to the bedroom and it started with its 3 vibrations, signaling a low BG. A finger stick confirmed – 49. I had a juice box and waited a bit before trying to fall asleep. This was around 10pm. This 49 turned into a low that would not go up until 3am. That is a 5 hour low blood sugar. 5 hours. I had numerous juice boxes, decreased my basal first by 20%, then by 50% and finally by 80%. In all my years of living with diabetes I will never understand what causes persistent lows like this. You would think after a couple of hours, my liver would have gotten the hint for some glucagon! Maybe the exercise had something to do with it, however I should have had enough carbs in my bloodstream to compensate for it. I have also been exercising a few times a week so it shouldn’t have been a shock to my body. At one point, I was on the verge of tears wishing for God to please make the low stop. All I wanted to do was sleep. I am very thankful to have had my Dexcom. Although its alarms every 30 minutes was what was keeping me awake, I otherwise may have just fallen asleep and not able to stay on top of that darn low.
And of course since diabetes is a bitch, I have been around 200+ mg/dL since I woke up this morning. Needless to say, I am feeling like a zombie today. I’m already thinking of later tonight when I get home and can hopefully go to sleep early. Nonstop lows are bad enough during the day. But they are so much worse during the night, when you’re supposed to be sleeping.
Not Always as Easy as Insulin.
On Christmas eve, we held a small get together at our place. We had enough food for about 25 people when there were only 6 of us! Even though I hadn’t indulged too much, my BG soared to about 250 mg/dL around dinner time. There was a delicious red velvet cake to be eaten afterward and I was upset that I was going to have to pass at the moment because of my high BG. One of my friends asked how long I would have to wait for it to come down. I told him it depends but it could possibly take a while. This got me thinking of how intricate managing glucose levels really is. To an outsider, it may seem like if a person with diabetes’ blood sugar is high they would take insulin and it would come back to normal promptly. Not always the case.
Then this morning, Scott pointed out a great post from Alexis over at I Run on Insulin. She talks about the complexities of managing BG more from the liver’s perspective but it resonated with me because of what I was thinking about a few days ago. Insulin is not the only thing missing from a person with diabetes’ body. Back when I was diagnosed, this wasn’t really part of the education given. We were taught to give daily insulin injections and sent on our merry way. But there are other hormones and functions affected by that attack of one’s beta cells. Science is not my thing. I work in Finance for Pete’s sake! I’m not going to pretend to completely comprehend the biology of it all but I do understand that insulin is not the only thing that regulates glucose from the blood to the body’s cells. There is glucagon which is another hormone secreted by the pancreas that causes the liver to convert stored glycogen into glucose when the blood glucose level is too low. Glucagon and insulin work together to keep glucose levels stable. And there is amylin, a partner of insulin. It is secreted in response to meals in order to maintain glycemic control.
In a person with diabetes, all three of these hormones do not work properly, if at all. Add that to the variables of taking human made insulin, through human made devices based on non perfect, human made decisions, it’s a wonder how our blood glucose levels are ever near normal! It’s never not always as easy as insulin.